Abstract
Introduction:
Integrative hematology oncology (IHO), the combination of complementary medicine in conjunction with conventional cancer treatments, is emerging as an important supportive care modality. Formal education programs, such as IHO fellowship programs, are not currently available. We conducted a national survey to gauge interest and investigate barriers to the development of IHO training programs in the US.
Methods:
An 18-question survey was sent to hematology/oncology, radiation oncology, and palliative care program directors, physicians, and fellows, and internal medicine residents planning to enter into any of the above fellowship programs. Recruitment was national with use of public email list servs and social media. Program directors and fellowship programs were identified through the Accreditation Council for Graduate Medical Education (ACGME). Participant informed consent was completed online and, Qualtrics survey links were shared weekly via email in two 4-week sessions.
Results:
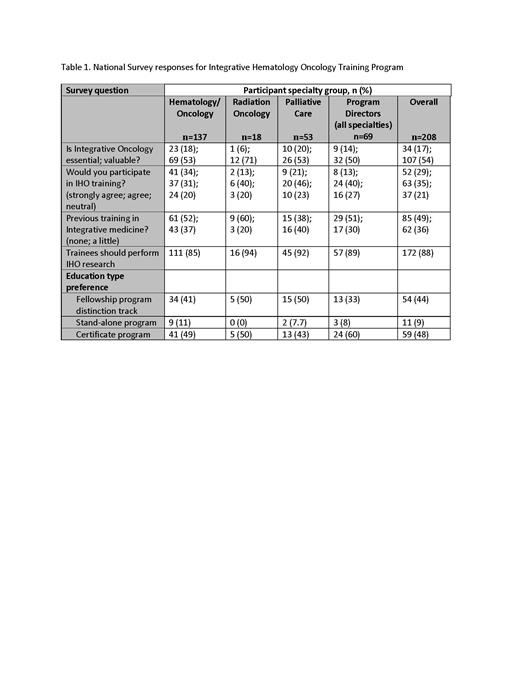
Participants (n=208) included physicians from: Hematology/Oncology 65.9% (n=137), Radiation Oncology 8.6%(n=18) and Palliative Care 25.4% (n=53). Hematology oncology respondents included physicians 47.4% (n=65), fellows 33.6% (n=46), and residents planning to enter into a hematology oncology fellowship 3.6% (n=5). Program directors (n=69) from each specialty included: 15.3% (n=21) from hematology/oncology, 61.1% (n=11) from radiation oncology, and 69.8% (n=37) from palliative care. Interestingly, palliative care had the highest response rate in this category. Survey respondents were mostly aged 31-40 y (38.4%), 41-50 y (23.8%), or 51-60 y (21.5%). Participant genders were male (45.7%), female (50.9%), or prefer not to identify (3.5%). There was diverse regional participation across the United States. Overall participant responses revealed significant interest for an IHO training program, despite little (36.0%) to no (49.4%) previous training in integrative medicine (Table 1).
Curriculum topics of primary interest were physician/provider wellness, stress reduction techniques, off-label use of medication, exercise/physical activity, nutrition, and lifestyle counseling. The preferred education delivery was didactic lectures and clinical practice exposure. Barriers to implementation included lack of good curriculum and inadequate budget/time/faculty experience to implement the program. Need for IHO training was based on perceived benefit to patients in 39 participants (73.6%), and patient request for services in 37 participants (68.8%).
Conclusion:
In this national survey of 208 physicians, the majority (64%) expressed interest in IHO education programs. Barriers included lack of curriculum, expertise, budget, and time. Education preference for fellowship track and certificate programs were similar, suggesting interest of both available options. Most participants (87%) felt fellows should participate in IHO research. In conclusion, IHO training is perceived as valuable and desirable. Thus, the development and dissemination of IHO training programs is needed.
Gowin: Incyte: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal